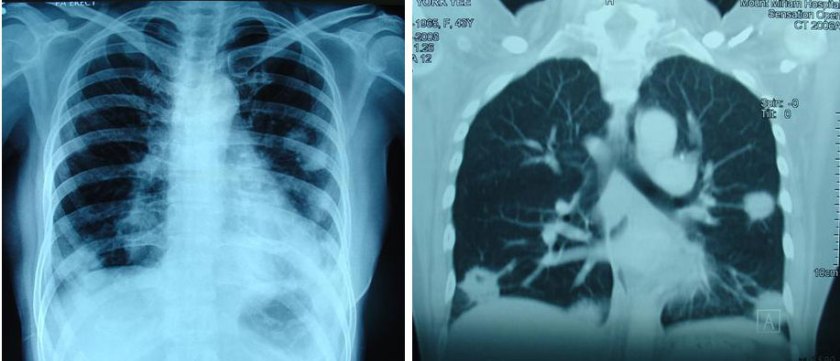
Tin (M597) was 38 years old in 2007 when she found lumps in her breasts during a regular medical check up. A CT scan done on 21 May 2007 indicated: no lung nodules or abnormal masses or enlarged lymph nodes. In the left axilla are slightly prominent lymph nodes – these are under 1 cm in size. There are no liver lesions seen.
Tin underwent a left mastectomy on 1 June 2007. The histology report indicated:
- Right breast biopsy – fibroadenoma in background of fibrocystic disease.
- Left breast (biopsy and mastectomy specimen): multifocal ductal carcinoma in-situ with invasive ductal carcinoma; invasive carcinoma measures 4.3 cm in maximum diameter; DCIS and invasive carcinoma extend close to the deep resection margin; skin and nipple are not involved by tumour.
- Left axillary lymph nodes: 4 out of 6 lymph nodes contain metastatic carcinoma, with extracapsular spread.
- TNM classification: pT2N2aMx, Stage 3A.
The tumour is negative for oestrogen and progesterone receptors, weakly reactive to C-erb-B2 and strongly reactive to P53. These results suggest that the breast cancer is unlikely to respond to tamoxifen / endocrine therapy.
As with most cancer patients, Tin underwent chemotherapy and radiotherapy after the surgery. Her husband was not sure how many courses of chemotherapy Tin had received. But one thing was sure – she was not getting any better. The oncologist behaved gently and encouraged Tin to continue taking the chemotherapy in spite of her deteriorating condition. She had full faith in her oncologist. According to her husband, Tin received Avastin towards the end of her chemo-treatment. Tin also underwent radiotherapy but her husband could not remember how many times she received the radiation treatment.
A follow up CT scan on 14 May 2008 indicated: no lung nodules or masses seen. Mediastinum remains clear of mediastinal lymphadenopathy. Liver also remains clear of metastatic deposits.
CT scan on 17 February 2009 indicated:
- Multiple pulmonary metastases are noted. This shows interval increase in size and number when compared with previous CT dated 22 December 2008.
- There is also interval development of bilateral pleural effusions, left larger than the right.
- Mediastinal and bilateral hilar lymphadenopathy are seen. This is unchanged when compared with previous CT. There is however interval development of left axillary nodes.
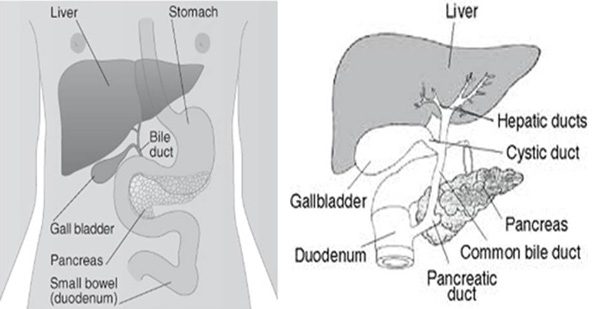
- There are now several small subcentimeter hypodense lesions seen in the liver compatible with hepatic metastases. These are not present in the previous CT.
CT scan on 8 June 2009 indicated:
- There is extensive pleural shadowing seen in the lung fields on both sides with evidence of associated effusions noted.
- This is associated with lung nodules in both lungs the largest of which measures approximately 1 cm in the mid zone of the left side.
- A small associated pericardial effusion is seen.
- In the lower cuts, the liver outline shows no abnormalities.
Tin’s husband and mother-in-law came to seek our help on 2 July 2009. This is the gist of what we were told.
Tin’s husband and mother-in-law did not seem to agree that Tin undergo such extensive medical treatment but Tin insisted in carrying out what the oncologist wanted her to do. She questioned:Herbs are not proven, what if I took herbs and these do not work. As a result, her mother-in-law was afraid to give further comment. Even when Tin’s condition had turned worse and she became breathless due to fluid in her lungs and pericardium, the oncologist was saying there was nothing to worry. Every three weeks she had to have a blood transfusion. After Tin gets out of the hospital, the oncologist said she should come back to him for more chemotherapy.
Realizing that she was not going anywhere with medical treatment, Tin as last agreed to try our herbs. This resulted in Tin’s husband and mother-in-law flying to Penang to see us. We prescribed some herbs but expressed our skeptism.
On 19 July 2009, Tin’s husband came to Penang again. He informed us that Tin had been hospitalized and was only able to take the herbs for three days so far. Her condition was deteriorating. The doctor had requested the family to take Tin home. At most she would survive for another 2 months. Tin needed oxygen to help her breathe.
All in all, the family had spent approximately S$200,000 for the treatment. Tin’s husband told us: Please try to save my wife.
Barely 3 days after her husband’s second visit, we received this e-mail:
Wed, Jul 22, 2009 at 5:42 PM
Dear Mrs Teo,
Thank you so far for your help rendered by you and Dr. Teo. This morning at 9:21 am, my wife finally passed away after her struggle against the cancer for this past 2 years. She lost her battle ….
Comments: Is losing a battle against cancer such as this something unusual? Definitely not. At CA Care we witness see such disasters all too often. Tin had undergone all the medical treatments necessary for cancer and she died within two years. Where is the proven science in this case?
Granted, Tin’s cancer was serious – Stage 3A, but her CT scan of 14 May 2008 indicated no problem with her lungs or liver. There were also no serious problems with her lymph nodes. But one a half years later, trouble started brewing. CT scan in December 2008 indicated recurrence and it became even more serious in February 2009 in spite of more treatments (more of different poisons?).
By June 2009 Tin’s condition became more critical and she had fluid in her lungs and also her pericardium (heart lining). What had happened? Was this due to her cancer or the results of her treatment?
Often treatments of breast cancer are referred to as Slash, burn and poison. It is also said that these treatments are worse than the disease. What could have happened if Tin were to do nothing invasive and go for alternative treatment? Having to suffer and to spend S$200,000 but ending up dead within 2 years is no bargain at all.
Dr. Frank Daudert of Pro Leben Klinik in Igls /Innsbruck, Austria said: Doctors give chemo, chemo, chemo. And patients die, die, die. He went on to say: Doctors are blindly giving chemotherapy to some patients while the cancer cells smile and the patients die.
Tin was totally committed to curing her cancer by the medical way. To her, herbalists are quacks and the herbs are not proven. She had resisted seeking alternative therapy or help. According to her family she only agreed to take the herbs in July 2009, and a few days later she died. That was a bit too late! There are many patients who are like her. Let this be a lesson to numerous others who come after her.







You must be logged in to post a comment.