Case 1
Fay (not real name) is a 45-year-old Malaysian. She was diagnosed with breast cancer in September 2006.
- She underwent a mastectomy with axillary clearance (removal of lymph nodes).
- After the surgery she received 25 radiation treatments and six cycles of chemotherapy. The drugs used were 5-FU, epirubin and cyclophosphamide (FEC). All treatments were completed in April 2007.
- Every 4 months Fay went back to her oncologist for routine surveillance check up. Everything was alright.
- In August 2008, cancer was found in her bones – L2, L5, sacrum and pelvis.
- She had been on tamoxifen for almost 2 years (November 2006 to August 2008). Tamoxifen had failed and the doctor suggested that she take another drugs, Arimidex.
- She received to receive more chemotherapy and suffered badly from the side effects.
Case 2
Rin (not real name) and is a 40-year-old Indonesian lady living in the United States. She wrote:
- First I was diagnosed with breast cancer in December 2004.
- I did the lumpectomy on the left breast in February 2005.
- After the surgery, I received 8 cycles of chemotherapy. After the chemotherapy I had menopause.
- I then had radiotherapy for 35 times and I finished it in October 2005.
- I took tamoxifen, 20 mg once a day.
- I did regular check up with my oncologist every 6 month and I did yearly mammogram and the past 2 years I also did the bone density test.
- In August 2008, I started feeling pain in my left leg and sometimes in my left arm. The pain did not go away and it hurt more and more. Then I was not able to and walk straight and could not bend. It was very hard for me to go up and down the stairs.
- In November 2008, I had a whole body scan and also CT scan. The cancer had spread to the bones – left humeral head, left femur and L5.
- I again did radiotherapy for the effected area for 10 times.
- In Dec 2008, I developed blood clots in my left leg.
- My doctor changed my medication from tamoxifen to Arimidex.
Case 3
Gay (not real name) is a 43-year-old Australian. She was diagnosed with breast cancer in 1999. She wrote:
- I received 6 months of chemothrapy and 3 months radiation therapy.
- Then I was started on tamoxifen for 5 years followed by Arimidex.
- I have had no problems until the past 6 months. I had a slight pain in my right upper abdominal. My tumor markers were elevated.
- After a number of scans, it turned out to be bone metastases.
Case 4
Sri (not real name), 57-year-old Indonesian, was diagnosed with left breast cancer in 2003. She underwent a mastectomy followed by chemotherapy and radiotherapy. At the time we talked to her, Sri appeared to have chemo brain and was unable to recollect the details of her treatment. Her response to our questions was also very slow. Sri received all these treatments in New Zealand.
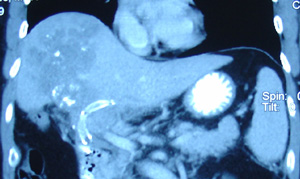
Sri went back to her doctor for routine check up and was told everything was fine. However, in 2007, she did not feel well. Further examination indicated bone metastases. She again received six cycles of chemotherapy and 10 radiation treatments. All treatments were completed in November 2008. Sri came to Penang in February 2009 and did a CT scan. The results indicated the following:
- Lesion in T1 and T5 vertebrae.
- Nodule in C5 and lesion in L4 vertebral bodies.
- Several lytic lesions in the left iliac bones.
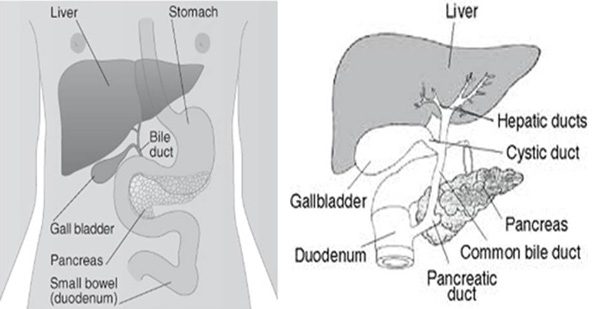
- Suggestive of liver cirrhosis.
What can we learn from these four cases?
1. These patients had undergone all the required medical treatments – surgery, chemotherapy, radiotherapy, and oral drugs – tamoxifen and Arimidex. They had received the best that medical science has to offer but cancer still recurs.
2. Oncologists say all these are treatments are scientifically proven, FDA-approved backed by data reported in peer-reviewed medical journals. The questions are: What is so great about all these? Why do these patients still suffer metastasis? What is the “real and honest” truth about all these treatments?
3. Does it ever cross somebody’s mind that the inability to cure or the ability of the cancer to spread could also be due to the treatments themselves?
4. Look at these cases again. Fay in Malaysia suffered metastasis 1 year and 4 months after completion of her medical treatment. Rin from USA and Sri in New Zealand suffered metastasis barely three years after her treatment while Gay from Australia had metastasis about eight years after her treatment. These cases reflect similar problems faced by most patients everywhere in the world. It does not matter where you live and who or what you are, doing the same thing produces the same results.
Einstein said: Insanity is to the do the same thing over and over again and expecting different results. Can you learn anything from the wisdom of this great Man of Science? Patients in the USA,Australia, New Zealand and Malaysia received the same kind of treatments and all of them ended up with the same results. Over the years, I have observed similar stories being repeated over and over again so much so that bony metastasis can or is expected after such treatments. To expect otherwise is what Einstein said is insanity.
The questions that boggle the mind are: Why are those in the know NOT doing anything about it?Why are patients kept in the dark and not warned about this possibility? Perhaps we can do MORE than just prescribing drugs? Tamoxifen is supposed to prevent recurrence but in all the cases above, it has failed miserably. Why don’t we look beyond what are being done today?













You must be logged in to post a comment.