As far as cure is concerned, there is no use pretending that brain tumours are truly curable ~ Dr. Jeffrey Tobias and Kay Eaton in Living with Cancer
In the first two weeks of January 2011, we encountered three brain cancer cases at CA Care.
On 1 Janaury 2011, we received this e-mail.
Dear Dr Chris,
We are based in Melbourne and came to know about CA Care through a close family friend in Kuala Lumpur. As we are unable to come there ourselves, the family friend will be visiting the centre with Z ‘s medical reports and scans.
Patient Full Name: Z Age: 4 years old
Gender: Female Cancer: Anaplastic Astroblastoma
Medical History:
Z started with headaches and neckaches in early 2010. We only notified the problem when her eyes and mouth cannot move correctly in around March 2010. We had been visiting few doctors, until she started vomiting in the morning, one of the doctor recommended to do a brain CT scan for her. It was done on the 12nd May 2010. Z was referred to Melbourne Royal Children Hospital immediately after the scan. A size of a tennis ball tumor was found in her brain. She had an urgent brain surgery on 15th May 2010. The surgeon and the oncologist suggested radiotherapy and chemotherapy, but we refused to do so. We putted her on Bill Henderson’s cancer free diet since June 2010. Unfortunately her tumor re-grows. Now the surgeon and oncologist recommended the same thing again, surgery and radiotherapy. But we refused to do surgery immediately.
On 13 January 2011, was another e-mail.
Hi Chris,
My name is J. I am contacting you from Adelaide, South Australia. My father has got a brain tumour and has had it since 2004. He has undergone three operations along with radiotherapy and chemotherapy treatments and is now looking for other treatment options. He mentioned to me that he heard that there is other treatment offered in Indonesia and asked me to investigate. What are your thoughts about the treatment you offer and if you think it’ll be beneficial to my father, and what is the process in commencing this treatment.
On 9 January 2011, we received this e-mail.
Hi Dr. Chris Teo,
We are coming to see you from Kuala Lumpur today. We should reach your office around 7 p.m.
Surgery was done on 15 November 2010. This cost RM 50,000. According to the surgeon only 60 to 70% of the tumour was removed. The histology is that of a sPNET (supra-tentorial primitive neuro-ectodermal tumour). No chemotherapy or radiotherapy was indicated after the surgery.
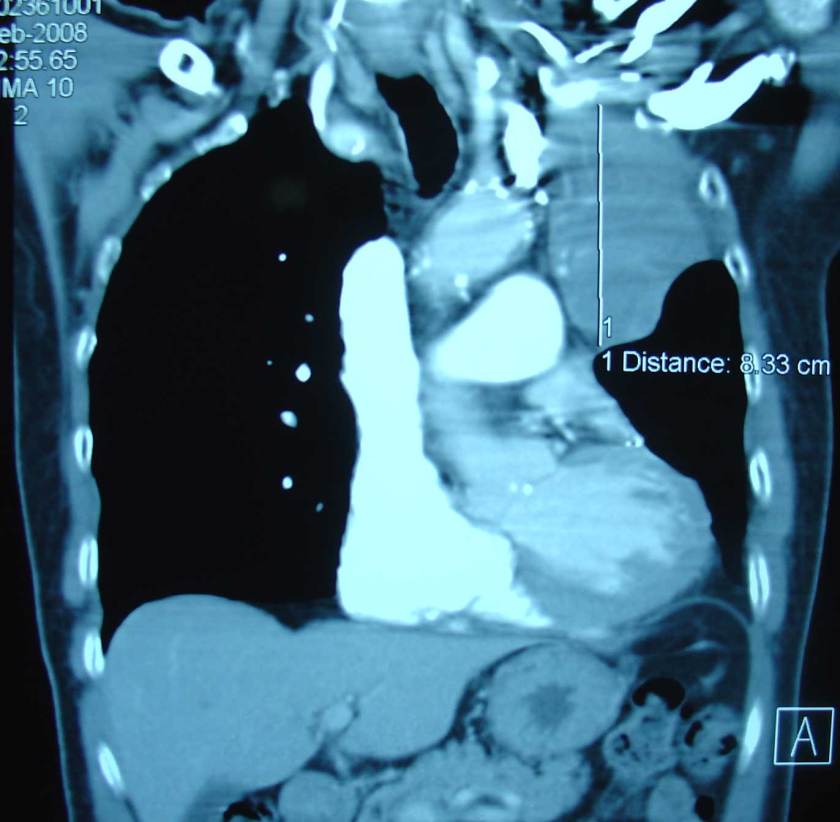
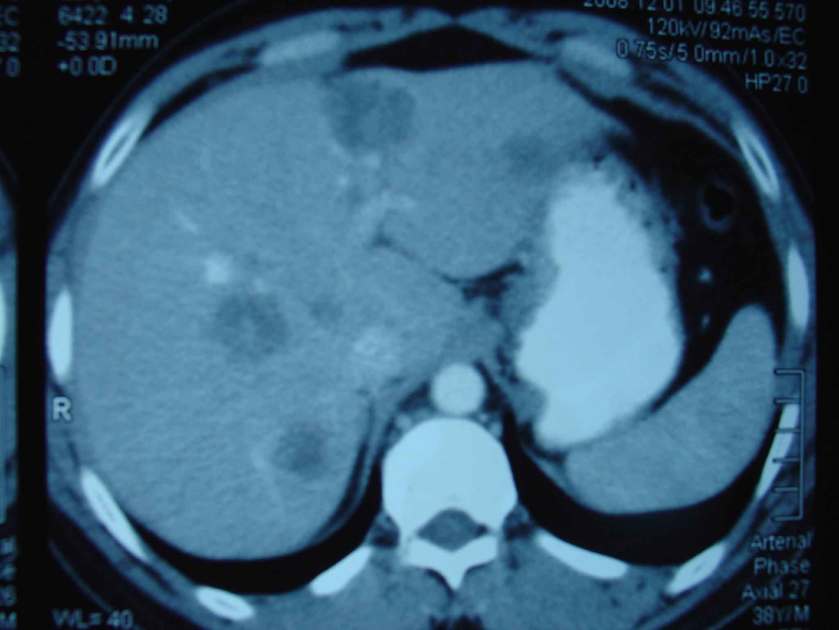
MRI done on 6 December 2010, i.e. about three weeks after the surgery, still showed a very large residual tumour, 8 x 7 x 6 cm, in the left parieto-temporal lobe extending to the thalamus.
A neurosurgeon in one private hospital was of the opinion that a second surgical resection could safely be done. The parents were reluctant to agree to this. The treatment plan after the proposed second surgery is craniospinal radiotherapy (CSI) followed by four consecutive courses of high-dose chemotherapy with autologous stem cell rescue (ASCR) each time, i.e. four tandem autologous peripheral blood stem cell transplants over a four to five month period.This procedure would cost about RM 200,000.
The parents were told that there could be a 50 to 70% chance (whatever that means?) if the residual tumour is first removed to about 10% of its size. The procedure carries a risk of causing some degree of handicap.
The parents went to Singapore for a second opinion. They were told by the Singapore surgeon that a second surgery could be done with good chance recovery (whatever that means again!). The operation in Singapore would cost S$60,000.
The Bench Mark: Heroic Acts by an Outstanding Neurosurgeon
Whenever I come across brain cancer cases in CA Care, I cannot help but remember the book, The Scalpel and the Soul written by Dr. Allan Hamilton – a neurosurgeon at the Arizona Health Sciences Centre, USA. Dr. Hamilton wrote a great book and I greatly admire him. Let me highlight some of the brain cancer cases that Dr. Hamilton wrote about. There are many things we can learn from these stories. Let these stories be the bench mark upon which you base your decisions when it comes to brain cancer.
Story 1: Anaplastic Astrocytoma
Taylor was a 18-year-old female and the daughter of Dr. Hamilton’s close friend, Candy. The entire left side of Taylor’s body had gone numb. Dr. Hamilton wrote:
“I was expert at using computer-guidance systems for neurosurgery, so I was not surprised that Candy asked me to do the biopsy procedure.
This kind of biopsy is dangerous – there would be little margin for error.
We would need to enter the brain in a relatively posterior location and then skirt past the motor cortex, where all the muscle coordination for the body lies. Then we’d have to slip seamlessly through millions of motor cell cables and sensory cells to gain access to a structure called the pulvinar. This was where the tumour seemed to have its epicenter. We plotted four different trajectories … and looked over on the computer.
The team had done hundreds of biopsies together, but this was definitely going to be one of the most challenging cases. There was little doubt we would get the job done, but could we get it done right?
One of the advantages of computer guidance is that you know within a millimeter exactly where you need to drill through the skull. In fact, the incision of this kind of surgery is less than half the width of the nail on your pinky finger. We close it up with a single stitch and cover it with one of those dot Band-Aids, so I could assure Taylor she wouldn’t lose any hair. No one would even be able to see the incision unless she pointed it out.
The news from neuropathology was not good. The tumour was an anaplastic astrocytoma – a high grade malignant brain cancer. And inoperable. We’d to depend on radiation and chemotherapy.”
Chemotherapy-Radiotherapy
“This young woman became bald, bloated and acne-ridden. Taylor was transformed in front of my eyes. It was like being in a horrible fairy tale where a spell is cast upon the beautiful princess.”
Worse news: the tumour did not respond. MRI showed clearly that the tumour was growing ever larger despite all our therapies and best intentions. Taylor died less than two months later.”
Story 2: Malignant Glioma
Alfred was thirteen years old when he felt that his right arm and right leg were not functioning properly. Something must have gone wrong in his brain. A CT scan and MRI showed a large tumour in his brain stem – no doubt a malignant glioma.
Dr. Hamilton wrote:
There are few procedures in neurosurgery more daunting than getting a biopsy of the brain stem – because it’s so full of important neurological functions. We call it “tiger country.” There’s hardly a surgical move that doesn’t hurt the patient. Even a piece of tissue no larger than the tip of a ballpoint pen contains some vital function. There’s no such thing as a safe brain stem biopsy – just a less dangerous one.”
This was what Dr. Hamilton did:
“The patient is affixed to a precisely machined head ring … It’s attached … by four pins directly to the bone of the skull. It must be absolutely unmovable. The patient then undergoes CT and MR imaging. A sophisticated software program allows the surgeon to pick out the target.
A tiny hole is drilled into the skull at the exact entry point picked up by the computer program. A foot-long probe is slid into postion. It passes down through the substance of the brain stem, almost to the hilt. The patient is awake so that brain stem function can be assessed.
Each time the probe moved into position, Alfred’s speech would become noticeably slurred. From the computer coordinates … I carefully took a small piece. When I withdrew the biopsy cannula, Alfred’s speech immediately cleared, returning to normal.
Afred was a little groggy when we finally removed the head ring …. treatments in less than eight hours.”
Chemotherapy-Radiotherapy
“Alfred underwent the usual six-week course of radiation treatments. As always, this was followed by a long course of chemotherapy and steroids. His hair fell out. His weight, under the incessant appetite stimulus of steroids, ballooned up to nearly two hundred pounds. He also broke out in a raging case of acne from the steroids. Another brain tumour-induced disfiguration before my eyes.
The tumour resisted everything we threw at it. Alfred lost control of his legs.
Alfred died. He eased into death with a little morphine.”
The only substantive thing I did was to ensure that Alfred’s dog could cuddle next to him in bed. The dog was smuggled into the hospital room in a large shopping bag. When the nurse discovered it, I wrote an order in the chart: “Dog to be at patient’s bedside every nursing shift – no exception.”
Story 3: Glioblastoma multiforme (GBM)
Donald was a twenty-three year old truck driver. He suffered from pounding headache that soon became a daily event. Often the headaches came on with nausea. The sunlight on the road and reflection off the windshield bothered him. CT showed a peach-sized tumour in the back of the brain – in the occipital lobe. The tumour caused a significant amount of swelling and pressure on the brain.
Dr. Hamilton wrote:
“After six hours of surgery, the tumour was removed. He made excellent recovery and was eating breakfast the morning after. He was discharged two days later.
What followed was six weeks of nonstop radiation therapy delivered every single day. I saw Donald lose his hair. I saw the grinding fatigue set it. The circles beneath his eyes. As soon as the radiation was finished, we launched into an aggressive regimen of chemotherapy for another six weeks. It was a marathon.
One thing I’ve learned over the years is that every tumour is different. Every tumour is nature’s experiment of one.
GBMs are almost never cured. Only five out of five thousand patients with GBM had survived five years or more. The odds of being a long-term survivor were exactly one in a thousand. But the bottom line is that GBMs are usually incurable. You never get to stop the treatments – the only way to hold this tumour at bay was to keep pounding away at it.
Donald was put back on another three rounds of chemotherapy. We also hit the centre of the tumour cavity with the intense single-fraction radiatioin of “radiosurgery.”
For the second year, Donald’s scan appeared reasonably dormant. The tumour seemed to be in remission.
In the third year, however, the tumour did return. With a vengeance. It was like a creature that had been wounded, had gotten up and was now stalking him … the tumour was growing rapidly.
I reviewed the scans. We would need to start a new line of aggressive therapy. We also decided to resect as much of the solid tumour as we could. So once again, I would have to go back into Donald’s brain and attack the tumour surgically.
Following surgery, he threw himself with total concentration into the next round of energy-depleting chemotherapy. Within three months, the tumour’s spread was clogging the flow through the ventricles … we made the decision to take Donald to the operating room and relieve the obstruction.
The operation took an hour and a half. I installed a device called a ventriculoperitoneal shunt (VP-shunt). By the end of the surgery, Donald was wide awake. He was back as bright as a brand-new penny.
Because the tumour was still growing, we turned to more experimental, far-out chemotherapies.
Over the next three months …. the shunt was keeping him out of life-threatening danger. In the spring – on April Fools’ Day – the shunt malfunctioned. It was completely blocked – tumour cells were growing inside it. Donald sank into a coma.
The day after surgery, Donald was already eating and asking to go home. The next morning Donald’s mother called me. She was sobbing. Donald had expired during the night. He was gone. “
Story 4: Glioblastoma multiforme – A Failure
Sidney (Sy) is Dr. Hamilton’s colleague. He was one of the United State’s outstanding Alzheimer’s disease specialists. He had a large brain tumour – the dreaded GBM. Dr. Hamilton described this case was “one of my most public failures in my career as a neurosurgeon.” This is how the story goes.
“The tumour had grown into his speech area. For me, it was paradoxically dreadful. I could end up making things worse. The risk was I might actually destroy his speech capacity in the process of removing the tumour.
Before any big surgery case, I have a ritual. I wake up early. I turn on the shower, steaming hot. I climb in and let the water wash over me for a few minutes. I wash my hair, my body, my face and last my hands. Then I remain under the shower and visualize the whole surgery in my heads. It’s as if I’m already in the OR (operation room). I visualize my OR team there. I watch myself do the operations … the operation seems to roll like a movie behind my closed eyes as I stand there in the shower.”
The Surgery
“It took almost two hours from when we removed the tumour to when we finished reconstructing the skull and closing all the layers of muscle and skin. I wheeled Sydney back to the recovery area.
Sy could process and understand speech perfectly, but he couldn’t utter a single word. My inner state was stark and miserable. I had failed Sy. My skills had failed us both. I didn’t have a choice. I had to sacrifice the small artery along with the tumour wall … I knew that … I might be sealing Sy’s fate. I wondered if we would ever be able to say another word. If not, it would be my doing.
I suppose I could rationalize that I’m not responsible for the patient’s anatomy. But it was my hand. My agony persisted In silence. Months later, when the tumour reappeared, none of us even mentioned surgery. Sy lived for another eight months.”
Dr. Hamilton wrote:
“There’s no loneliness like the solitary shadow that comes into a surgeon’s heart when he or she suddenly realize an irreversible error has been committed. You can make a mistake, hurt someone profoundly and not be able to go back and undo your error. The brain simply has no genetic capacity to regrow itself. One mistake and it’s all over. It’s the grace and curse of neurosurgery. “
Two Success Stories
Dr. Hamilton wrote:
“Much of my neurosurgical practice is devoted to brain tumours. I’ve had the honour of taking care of hundreds of patients with astrocytomas, malignant brain cancers. Very few survive for more than a couple of years. As I mentioned, the odds for long-term survival can be a thousand to one. To be cured one needs to be lucky indeed – it’s a real long shot.
Thank goodness every neurosurgeon who deals with astrocytomas has at least some survivors. Without this handful of the lucky few … it would be difficult to keep going. As surgeons, of course we must often resign ourselves to our patients’ unfortunate outcomes.
I have two “home-run” astrocytoma patients. One’s named Rusty and the other Paul. They are different from each other.”
Story 5: The Story of Rusty
“Rusty was an alcoholic, chain-smoker and a ne’er-do-well person who attaches himself to women and convince them to live with him. He has brain tumour. Rusty would come into clinic with his latest girlfriend. Usually he reeked of booze and sometimes he was downright obnoxious. When he was drunk, he had a habit of hanging off my shoulder as if he was my best buddy. Or he’d come swaggering down the hall, yelling, “Hey, doc! How ya doin’?
How long do I have? He asked me directly. I can never give a clear answer to that question, because there isn’t one … a surgeon has to be careful not to extinguish the patient’s hope … but the fact was I’d never had a patient survive more than six weeks after an astrocytoma had spread to the opposite hemisphere.”
Rusty was about two years out from the time of his original diagnosis. He had lived with three different girlfriends during that interval.
After thirteen years, in 2003, when I saw Rusty again in clinic, his scan hadn’t changed one bit. He still drank excessively, but he settled down with his mom and became a pretty good cook for the two of them.
His tumour defied all logic. It seemed to have just gone to sleep.”
Story 6: The Story of Paul
“ Paul was an engineering student who had a malignant astrocytoma. I resected it a week later. The severity of subsequent radiation and chemotherapy forced him to suspend his studies for an entire semester. The following year, he returned to his master’s degree. On the final scans at the completion of treatment, there was no visibile trace of a tumour. He got married and started working on his Ph.D.
Paul’s scan remained pristinely clean of any recurrent tumour. He’d been able to finish up a very challenging doctoral dissertation. Our whole clinic staff attended his graduation. We threw a small party for him. There were five candles on the “birthday” cake one of the nurses had baked – one for each year he’d survived from his initial diagnosis. He was my first five-year survivor.
In 2003, Paul reached almost fourteen years out from diagnosis. He and his wife had just finished building a little place in the hills. That same year, Paul had a seizure. There was a new spot. It had never been there before. Paul had to come back and undergo a course of focused radiation, aimed at killing the tumour – now he was haunted by the notion that his tumour was stalking him, lurking among the shadows of his MRIs. Bidding its time. “
On reflection, Dr. Hamilton wrote:
“I have learned that luck, good or bad, can spell the difference between surviving and perishing. It can be the power behind a successful surgery or a frightening complication. We have to just accept it: patient and physician. I still struggle to learn from their examples. But I still experience moments – years after they have passed away – when I cry for some of them. And for myself. So few home runs.”
Comments
As said earlier, I have great admiration for Dr. Hamilton. I admired his expertise, his humility, his deep sense of connectedness with humanity, his dedication to his noble profession and patient and his compassion towards his patients. I say this in my heart. If your want to fight and get even with cancer – this would be the man who would help you with the battle of your life. I read again and again the words written by Dr. Hamilton above. I would like to say as loudly as I can: the world needs more surgeons like this great man.
Dr. Hamilton’s book opened my eyes to what modern, high-tech, brain surgery could do. The techniques and scientific tools are so impressive!
But let us not be caught up with impressive tools and technology. More importantly, we need a pair of wonder hands who could do things with compassion and love.
Then, ultimately, it is the results that count. At CA Care we too have the privilege to help patients with brain cancer. We do not have those magical tools – ours are primitive by any standard – just drink bitter, smelly herbs. The tools may be primitive but we too have scored a few home runs!
In our website we have documented the healing of:
Daisy of Indonesia, Sunan of Thailand, CT of Medan,and a twelve-year-old girl from Penang, using only herbs. For details click the appropriate links.
In closing, and when dealing with brain cancer, let us be reminded of what Dr. Hamilton said:
“One of the greatest secrets of surgery, which no mentor can teach, is knowing when to stop a surgical procedure, to call an end to it – when to keep pushing onward and when you’ve gone too far. So often, a surgical outcome depends on where to call a halt. When to let the patient recover from the intrusion. Because surgery is just that – an intrusion of the body. Getting out at the right moment is half of a successful surgical outcome.”
Quotation from: The Checklist Manifesto – how to get things right by Atul Gawande
We talk about our great saves but also about our great failures, and we all have them.
The question … to answer was why we fail at what we set out to do in the world.
We have just two reasons.
The first is ignorance – we may err because science has given us only a partial understanding of the world and how it works.
The second is ineptitude – in these instances the knowledge exists, yet we fail to apply it correctly.
Failure of ignorance we can forgive. If the knowledge of the best thing to do in a given situation does not exist, we are happy to have people simply make their best effort.
But if the knowledge exists and is not applied correctly, it is difficult not to be infuriated… philosophers gave these failures so unmerciful a name – ineptitude. Those on the receiving end use other words, like negligence or even heartlessness.








You must be logged in to post a comment.